|
An Anthrax Primer
NPR's Science Desk Answers Some Frequently Asked Questions
 How Anthrax Works How Anthrax Works
NPR's Richard Knox reports on new research showing how anthrax kills, and new ways to cobat the toxins released by the bacteria. Oct. 23, 2001.
 More broadcast coverage of the anthrax investigation. More broadcast coverage of the anthrax investigation.
• What causes anthrax?
• Where are the bacteria found?
• How do people get infected?
• Is anthrax easy to catch and spread?
• What are the symptoms?
• How long after exposure do symptoms appear?
• How is anthrax definitely diagnosed?
• How long does diagnosis take?
• How often does anthrax occur?
• Why do animals get anthrax more often?
• How deadly is it?
• How is anthrax treated?
• Can it be prevented? What about a vaccine?
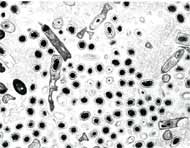 | |
Bacillus anthracis spores
Photo: Dept. of Defense |
What causes anthrax?
Anthrax is caused by a bacterium (not a virus). More specifically, it's a rod-shaped bacterium that stains purple in a laboratory test.
back to top
Where are the bacteria found?
The bacteria live in and on infected animals, and in the soil. The bacteria can't survive long in the environment when they're in a growth stage. But when they form spores -- which they do when the environment changes (for example, when they run out of food) -- they can live in the soil for decades.
back to top
How do people get infected?
There are three forms of anthrax: inhalation (where the bacteria lodge deep in the lungs), cutaneous (skin), and intestinal. By far the most common form is cutaneous (about 95 percent of cases).
• Inhalation anthrax comes from inhaling spores of anthrax bacteria. Spores work their way deep into the lungs, and are picked up by immune cells that carry them to lymph nodes, where they multiply and release poisons that cause hemorrhaging and other problems. Not all spores can set up an infection; they have to be small enough to work their way deep into the lungs. Also, 2,500 to 55,000 spores are needed to establish infection.
• Cutaneous anthrax occurs when anthrax bacteria are transmitted to humans from contaminated meat, wool or hides. They enter the skin, usually through cuts and abrasions; 95 percent of anthrax cases are cutaneous.
• Gastrointestinal anthrax comes from ingestion of contaminated, undercooked meat.
back to top
Is anthrax easy to catch and spread?
Anthrax is not easy to catch: Years ago, researchers tested workers in a goat-hair mill in Pennsylvania and found that workers regularly inhaled low concentrations of anthrax spores, yet didn't get sick.
And it's important to note: People do not transmit anthrax from one to another. It is not contagious.
back to top
What are the symptoms?
• Inhalation: Initially, flu-like symptoms -- aches, pains, fever -- developing into severe breathing problems, shock and death. It's not the same as cold symptoms; colds are marked by runny noses, and a runny nose is not one of the symptoms of anthrax.
• Cutaneous: raised itchy bumps that develop into ulcers with a black area in the center (hence the name anthrax, from the Greek anthrakis, meaning coal).
• Gastrointestinal: nausea, lose of appetite, vomiting, fever, abdominal pain, vomiting blood, diarrhea.
back to top
How long after exposure do symptoms appear?
There's some debate about this. The Centers for Disease Control and Prevention in Atlanta says within seven days. In an accidental exposure incident in the Soviet Union in 1979, cases occurred anywhere from two to 43 days after exposure. CDC's treatment recommendation is based on a possible 60-day window.
back to top
How is anthrax definitely diagnosed?
By isolating the bacteria from the blood, skin lesions or respiratory secretions.
back to top
How long does diagnosis take?
A variety of testing procedures are available; therefore, the time it takes to determine whether a person has been exposed to anthrax is variable.
According to an article in the Journal of the American Medical Association, a blood culture takes six to 24 hours, and will tell whether there's a general overgrowth of bacteria. Then technicians can do a "Gram test" where they apply special stains that highlight bacteria. A Gram stain takes 10 to 15 minutes, and will identify if the bacteria are in the same category as the bacteria that cause anthrax.
Biochemical testing that is specific to anthrax bacteria will take another 12 to 24 hours. The process can be shorter if anthrax is suspected. Sometimes diagnosis takes longer because transporting specimens to national reference laboratories can take time. Other bodily fluids can be tested, including spinal fluid.
back to top
How often does anthrax occur?
In a word, it's rare, at least in the United States. Sporadic cases occur in South and Central America, Southern and Eastern Europe, Asia, Africa, the Caribbean and the Middle East. Some public health experts believe that there may be a low level of cases in the United States that go undiagnosed, because no one looks.
Diagnosed cases on record:
• Inhalation anthrax: 18 documented cases in the United States from 1900 to 1978, mostly in agricultural workers.
• Cutaneous anthrax: 224 cases in the United States from 1944 to 1994.
• Gastrointestinal anthrax: NPR could find no reports of gastrointestinal anthrax in the United States; there were 14 cases in Thailand in 1987.
In other countries, cutaneous and even inhalation cases are more common. And animal outbreaks are more common than that; Canada recently had one.
back to top
Why do animals get anthrax more often?
Cattle and other grazing animals are constantly disturbing the soil as they eat, dispersing anthrax in the immediate area of their noses. Likewise, spores adhere to animal hides through contact with spores in soil and the environment. Animal handlers, including veterinarians and ranch hands, are usually vaccinated against anthrax due to the risk of cutaneous anthrax (and, to a lesser extent, inhalation anthrax).
back to top
How deadly is it?
• Cutaneous: 20 percent fatality rate (without appropriate antibiotic treatment).
• Gastrointestinal: 25 to 60 percent fatality rate (even with appropriate antibiotic treatment).
• Inhalation: Fatality rate estimates range from 80 percent to 95 percent (even with appropriate antibiotic treatment). One reason estimates vary is that the numbers are based on people who got sick decades ago, before the development of critical care units. Some researchers think supportive medical therapy (fluids, etc.) might be effective in some cases. Nearly half of all deaths occur within 24 to 48 hours of serious symptoms.
back to top
How is anthrax treated?
Anthrax can be treated in its earliest stages with penicillin (often delivered intravenously), ciprofloxacin (brand name, Cipro) or doxycycline. Evidence of antibiotic effectiveness comes from use in humans and animals. Other antibiotics related to ciprofloxacin may work as well. Other antibiotics -- including chloramphenicol, erythromycin, and some cephalosporins -- have been shown to kill anthrax in laboratory dishes, but there have been no animal studies of these drugs to date.
There have been a variety of reports, some more credible than others, that the Soviet Union developed a penicillin-resistant form of anthrax for use in biowarfare. That's one reason why doctors tend to prefer ciprofloxacin over penicillin. Also, Cipro is the only drug specifically approved by the FDA for treatment of inhalation anthrax exposure, although studies show that generic penicillin and doxycycline are as effective. But Cipro is not recommended for children, due to animal studies suggesting that it may affect bone growth.
Late-stage treatment of inhalation anthrax, after symptoms have developed, is supportive -- keeping blood pressure up, keeping the person breathing and hydrated. It has not been shown to be effective.
back to top
Can it be prevented? What about a vaccine?
An animal vaccine is available and widely used in countries where anthrax is common.
A human vaccine is available, but there are concerns about its routine use. The effectiveness of the vaccine is unclear. That's because it's tough to test a vaccine against a lethal condition -- you can vaccinate people, but it would not be ethical to test the vaccination's effectiveness by exposing people to anthrax. The CDC says the vaccine is 93 percent effective, based on real-world experiences.
The company created to manufacture it, BioPort of Lansing, Mich., has little experience in producing vaccines, and has been beset by multiple production problems. After the company suffered financial problems that threatened to end all American production of the anthrax vaccine, the U.S. Defense Department essentially took over the company and is in control of production and distribution. Even so, the FDA suspended shipment of human anthrax vaccine from this facility last year because the company violated manufacturing rules; NPR has reported that workers were adding unapproved ingredients to the vaccine even as FDA inspectors looked on.
The anthrax vaccine was used in the Gulf War. Some military personnel were concerned enough about the vaccine's safety that they refused it, and were disciplined.
The vaccine is what's called a cell-free filtrate, meaning it contains no live, dead or disabled bacteria. Multiple shots are needed. The CDC recommends three injections two weeks apart, then boosters at six, 12 and 18 months, with annual boosters after that.
back to top
Other Resources
• Centers for Disease Control and Prevention
• Journal of the American Medical Association
• Department of Defense Anthrax Vaccine Immunization Program
|